Conditions
- Home
- Conditions
Eye Conditions
We have specialists in all areas of ophthalmology. Our main interest is to provide the best care for your eyes and vision, using the most advanced technology.
The lens of the eye is normally clear and acts similarly to a camera lens, focusing the light as it passes to the back of the eye.
Until about 45 years of age, the shape of the lens is able to change. This allows the lens to focus on an object, whether it is near or far.
As a person ages, the proteins found in the lens start to decompose and, as a result, the lens become opaque.
What the eye sees may appear blurry. This condition is known as cataract. Factors that can accelerate cataracts to form are:
· Diabetes
· Inflammation of the eye
· Eye injury
· Family history of cataracts
· Prolonged use of corticosteroids (taken orally) or other medication
· Exposure to radiation
· Smoking
· Surgery due to another eye condition
· Too much exposure to ultraviolet light (sunlight)
In many cases, the cause of cataracts is unknown.
Symptoms
Cataracts develop slowly and painlessly. The vision in the affected eye also gets worse slowly.
- The slight clouding of the lens often occurs after the age of 60 but it may not cause any vision problems.
- By the age of 75, most people have cataracts that affect their vision.
Visual problems may include:
- Being sensitive to glare
- Cloudy, blurry or fuzzy vision
- Difficulty seeing at night or in dim light
- Double vision
- Loss of color intensity
- Problems seeing shapes against a background or the difference between shades of colors
- Seeing halos around lights
- Frequent changes in eyeglass prescriptions
Cataracts lead to decreased vision, even in daylight. Most people with cataracts have similar changes in both eyes, although one eye may be worse than the other. There are often only slight visual changes.

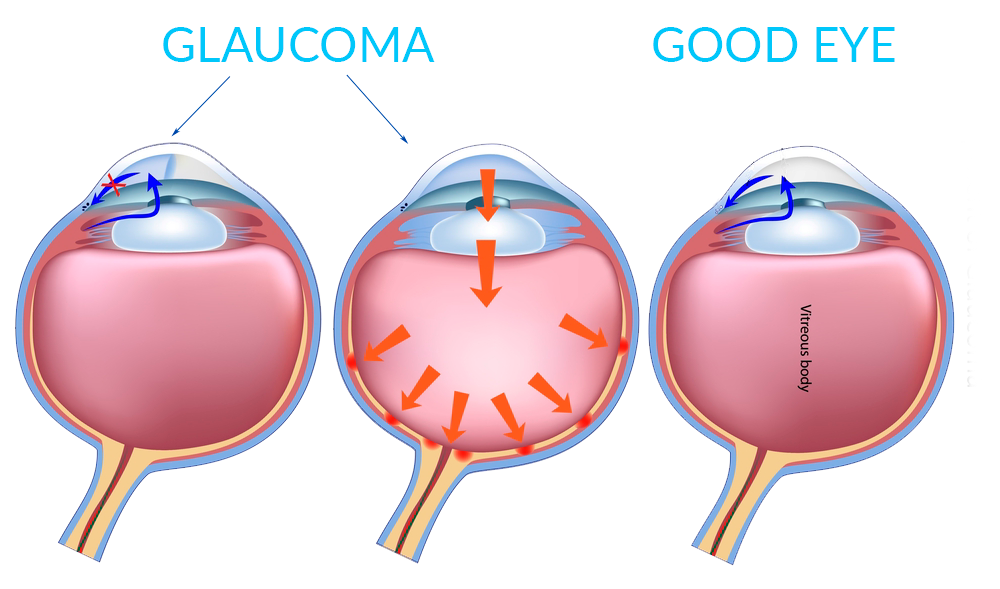
Glaucoma is a group of conditions that can damage the optic nerve. It is the leading cause of blindness in the United States. It usually occurs when the pressure of the liquid found inside the eyes rises slowly and damages the optic nerve. It is possible that there are no symptoms to begin with. Without treatment, people with glaucoma lose peripheral vision (side vision). They feel like they are looking through a tunnel. Over time, this tunnel vision (field of vision) may decrease until leading to blindness.
A comprehensive eye exam can determine if you have glaucoma. Some people are more at risk than others. These people should get a complete eye examination at least once every two years. Those at risk are:
· African Americans over the age of 40
· People over the age of 60, especially Mexican Americans
· People with a family history of glaucoma
There is no cure for glaucoma but it can be controlled. Immediate treatment during the first stage can help prevent loss of vision. Treatments usually include eye drops and/or surgery.
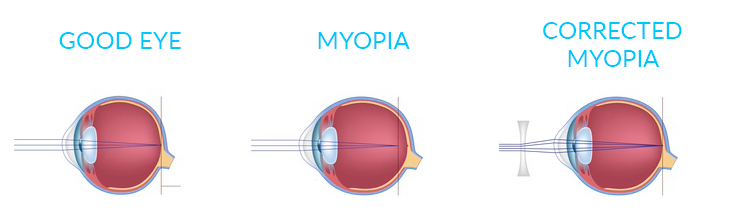
Nearsightedness, or myopia, occurs when the light entering the eye focuses incorrectly, making distant objects appear blurred. Myopia is a refractive error of the eye.
Causes
People are able to see because the front of the eye can bend (refract) light and points it to the back surface of the eye, called the retina.
Nearsightedness occurs when there is a discrepancy between the power to focus and the length of the eye. Rays of light focus in front of the retina instead of directly on it. Consequently, what you see is blurry. Most of the eye’s focusing power comes from the cornea.
Myopia affects men and women equally. People with a family history of nearsightedness are more likely to develop it. Most eyes with nearsightedness are healthy, but a small number of people with severe nearsightedness develop a form of retinal degeneration.
Symptoms
A nearsighted person sees close up objects clearly, but distant objects appear blurred. Squinting will tend to make far away objects seem clearer.
Myopia is often first noted in school-aged children or teenagers. Children often cannot read the blackboard but can easily read a book.
Myopia gets worse during the growth years. People who are nearsighted need to change glasses or contact lenses frequently. It usually stops progressing as a person stops growing in his or her early twenties.
Other symptoms may include:
• Eyestrain
• Headaches (uncommon)
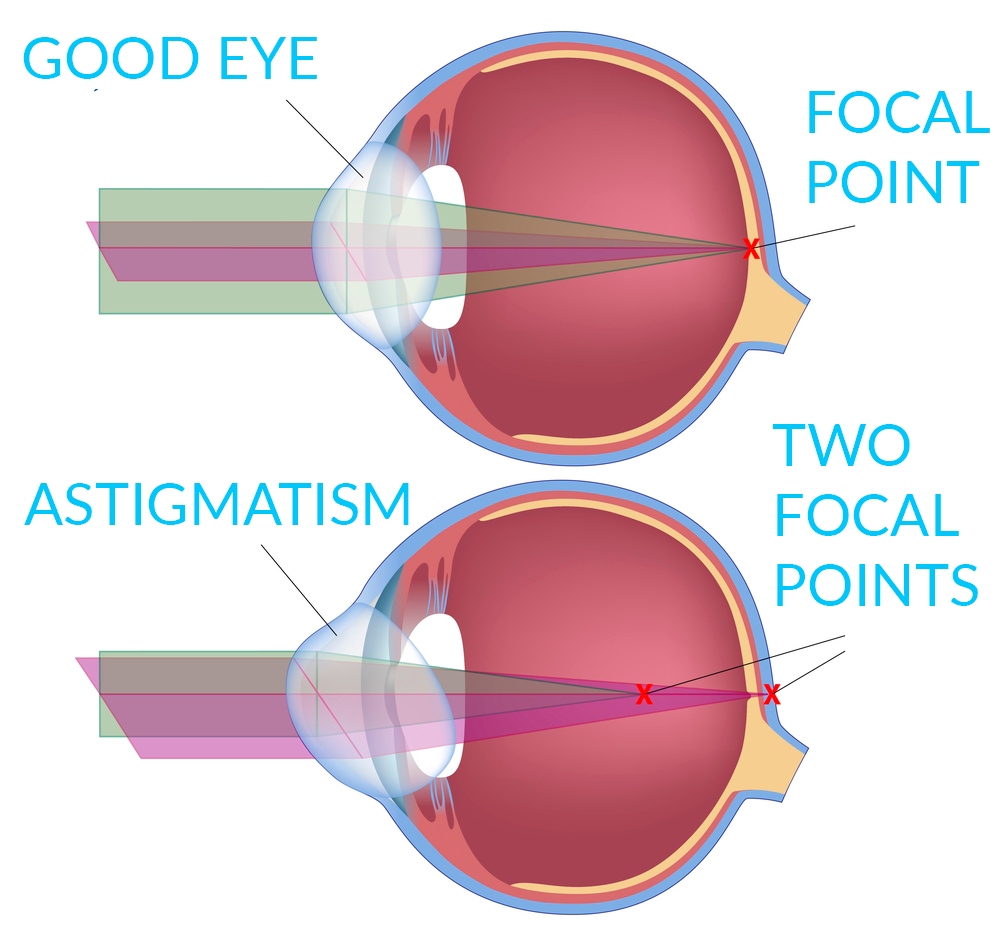
It is a type of refractive error of the eye. Refractive errors cause blurred vision and are the most common reason why a person goes to see an eye professional.
Other types of refractive errors are:
• Farsightedness
• Myopia
Causes
People are able to see because the front of the eye (cornea) is able to bend (refract) light and focus it onto the back surface of the eye, called the retina.
If the light rays are not clearly focused on the retina, the images you see may be blurry.
With astigmatism, the cornea is abnormally curved, causing vision to be blurred.
The cause of astigmatism is unknown. It is usually present from birth and often occurs together with nearsightedness or farsightedness. If the astigmatism gets worse, it may be a sign of keratoconus.
Astigmatism is very common. It sometimes occurs after certain types of eye surgery, such as cataract surgery.
Symptoms
Astigmatism makes it difficult to see fine details, either close up or from a distance.
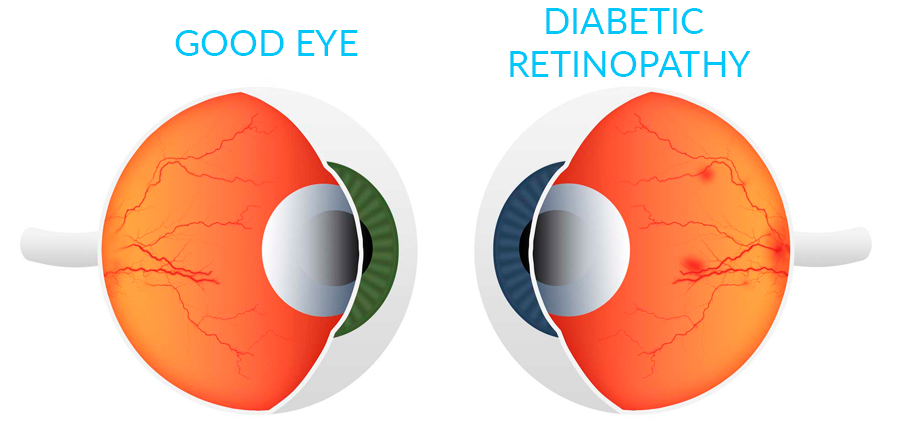
Diabetes can damage the eyes and damage the small blood vessels in the retina, the back of the eye, which is known as diabetic retinopathy.
Diabetes also increases the risk of glaucoma, cataracts and other eye problems.
Causes
Diabetic retinopathy is caused by damage to the blood vessels in the retina, the layer of tissue at the back of the eye. The retina changes light and images that enter the eye into nerve signals that are sent to the brain.
Diabetic retinopathy is the leading cause of blindness in Americans of 20 to 74 years old. People with type 1 or type 2 diabetes are at risk of having this condition.
There are two stages of diabetic retinopathy:
• The non-proliferative stage occurs first.
• The proliferative stage is more serious and advanced and is less common.
The probability of developing retinopathy and having a more severe form is greater when:
• You have had diabetes for a long time.
• Your blood sugar (glucose) in the blood has been poorly controlled.
Some types of exercise may worsen diabetic retinopathy. If you have retinopathy, consult your doctor before starting an exercise program.
Other problems that can occur in people with diabetes include:
• Cataracts: clouding of the eye.
• Glaucoma: increased pressure in the eye that can lead to blindness.
• Macular edema: blurred vision due to the leakage of fluid into the retina, which provides sharp, central vision.
• Retinal detachment: retinal scarring may cause part of the retina to pull away from the back of the eyeball.
Hyperglycemia or changes in the level of sugar in the blood often cause blurred vision. This is because the lens in the center of the eye cannot change shape when it has too much sugar and water. This is not the same problem as diabetic retinopathy.
Symptoms
Very often, diabetic retinopathy does not cause any symptoms until damage to the eye is severe. This is because the damage can affect an important part of the retina before vision is affected.
Symptoms of diabetic retinopathy include:
• Blurred vision and slow loss of vision over time
• floaters
• Shadows or missing areas of vision
• Difficulty seeing at night
Many people with early diabetic retinopathy have no symptoms before bleeding in the eye occurs. This is the reason why anyone with diabetes should have regular eye exams.
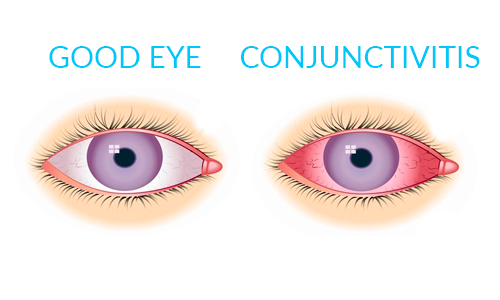
It is the swelling (inflammation) or infection of the conjunctiva, the membrane that lines the eyelids and covers the sclera of the eye.
Causes
The conjunctiva is exposed to bacteria and other irritants and tears help eliminate bacteria. Tears also contain protein and antibodies that destroy bacteria.
Conjunctivitis is usually caused by a virus. Viral conjunctivitis is called “keratoconjunctivitis” (pinkeye) and certain forms of it can be easily spread among children.
Other causes include:
• Allergies (allergic conjunctivitis)
• Bacteria
• Certain conditions
• Exposure to chemicals
• Chlamydia
• Mushrooms
• Parasites (uncommon)
• Use of contact lenses (especially extended-wear of contact lenses)
Newborns can be infected by bacteria in the birth canal. This condition is called neonatal ophthalmia and must be treated immediately to preserve vision.
Symptoms
• Blurry vision
• Scabs that form on the eyelid overnight
• Eye pain
• Gritty feeling in the eyes
• Increased lacrimation
• Itchy eyes
• Red eyes
Sensitivity to light
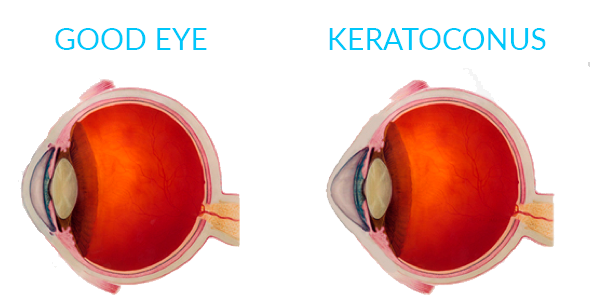
It is an eye disease that affects the structure of the cornea. The cornea is the clear tissue covering the front of the eye.
With this condition, the shape of the cornea slowly changes from the normal round shape to a cone shape. The eye bulges out which causes vision problems.
Causes
The cause is unknown but the tendency to develop keratoconus is probably present from birth. The condition may be due to a defect in the collagen tissue that provides shape and strength to the cornea.
Allergies and eye rubbing can accelerate the damage.
There is a link between keratoconus and Down syndrome.
Symptoms
The earliest symptom is subtle blurring of vision that cannot be corrected with glasses (vision can generally be corrected to 20/20 with rigid, gas-permeable contact lenses). Over time, you may have eye halos, glare and other night-vision problems.
Most people with keratoconus have a history of myopia, which tends to worsen over time. As the problem worsens, astigmatism develops.
Keratoconus is often discovered during adolescence but can also occur in older people.
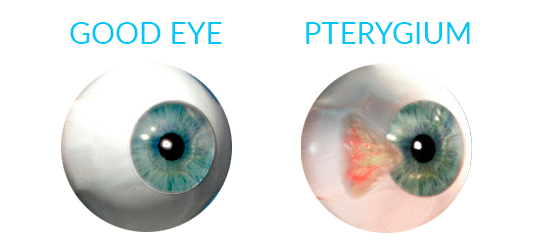
It is a non-cancerous tumor that starts in the thin tissue (conjunctiva) of the eye. This tumor covers the white part of the eye (sclera) and extends to the cornea. It is often slightly raised and contains visible blood vessels. The problem may occur in one or both eyes.
Causes
The exact cause is unknown. It is more common in people who are often exposed to sunlight or wind, such as people who work outdoors.
Risk factors are exposure to sunny, dusty, sandy or windblown areas. Farmers, fishermen and people living near the equator are often affected. Pterygium is uncommon in children.
Symptoms
The main symptom of pterygium is a painless area of elevated white tissue that has blood vessels on the inner or outer edge of the cornea. Sometimes the pterygium presents no symptoms. However, it may become inflamed and cause burning, irritation or the feeling there’s something foreign in the eye. Vision may be affected if the tumor spreads far enough onto the cornea.
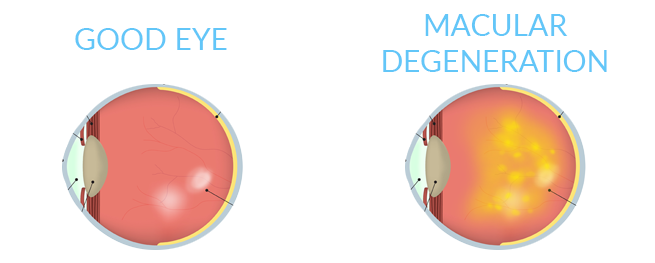
Macular degeneration is an eye disorder that slowly destroys the sharp, central vision, making it difficult to read and see fine details.
This condition is more common in people over the age of 60, which is why it is often called age-related macular degeneration (ARMD or AMD).
Causes
The retina is at the back of the eye and it changes light and images that enter the eye into nerve signals that are sent to the brain. A part of the retina, called the macula, makes vision sharper and more detailed.
Age-related macular degeneration (AMD) is caused by damage to blood vessels that supply the macula. This change also damages the macula.
There are two types of AMD:
• Dry AMD occurs when blood vessels under the macula become thin and brittle. Small yellow deposits, called drusen, form. Almost all people with macular degeneration have the dry form first.
• Wet AMD occurs in only about 10% of people with macular degeneration. New abnormal and very fragile vessels grow under the macula. These vessels leak blood and fluid. This form causes most of the vision loss associated with the condition.
Scientists are not sure what causes AMD. The condition is uncommon before the age of 55 and is most often seen in adults aged 75 and over.
Risk factors for AMD include:
• Family history of the disease
• Caucasian race
• Cigarette smoking
• High-fat diet
• Female gender
Symptoms
At first, you may not have any symptoms. As the condition gets worse, you may have problems with your central vision.
SYMPTOMS OF DRY AMD:
The most common symptom of dry AMD is blurred vision. Often objects in the central vision look distorted and dim and colors look faded. You may have difficulty reading print or seeing other details but can see well enough to walk and perform most daily activities.
As the condition gets worse, you may need more light to read or perform everyday tasks. A blurred spot in the center of your vision gradually gets larger and darker.
In the later stages, you may not be able to recognize faces until they are up close.
SYMPTOMS OF WET AMD
The most common early symptom of wet AMD is that straight lines appear distorted and wavy.
There may be a small dark spot in the center of your vision that gets larger with time.
With both types of AMD, loss of central vision can occur very quickly. If this occurs, you will need urgent evaluation by an ophthalmologist with experience in retinal problems.
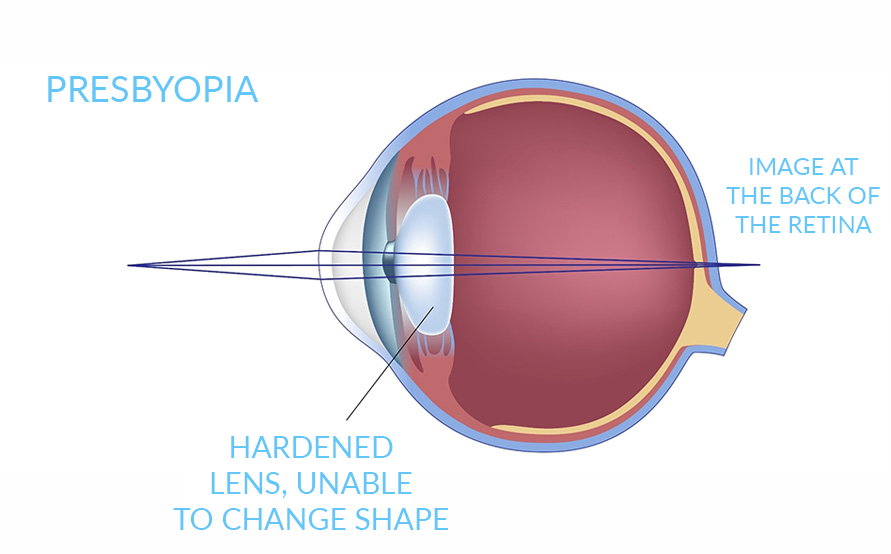
It is a condition in which the lens of the eye loses its ability to focus. This makes it hard to see objects up close.
Causes
In the young eye, the lens needs to change its length or shape to focus on close objects. The ability of the lens to change shape is called the elasticity of the lens and this elasticity is gradually lost as people age. The result is a slow decrease in the eye’s ability to focus on nearby objects.
People usually begin to notice this condition around the age of 45, when they realize that they need to hold reading materials further away in order to see properly. Presbyopia is a natural part of the aging process and affects everyone.
Symptoms
• Decreased ability to focus on close objects
• Eyestrain
• Headache
Presbyopia
Hardened lens, unable to change shape
Image at the back of the retina
It is a disorder in which the two eyes do not align in the same direction and, therefore, do not look at the same object at the same time. The condition is more commonly known as “crossed eyes” (convergent strabismus).
Causes
Six different muscles surround each eye and work “as a team” so that both eyes can focus on the same object.
In someone with strabismus, these muscles do not work together. Consequently, one eye looks at an object, while the other eye turns in a different direction and focuses on another object.
When this occurs, two different images are sent to the brain: one from each eye. This confuses the brain. In children, the brain can learn to ignore the image from the weaker eye.
If strabismus is not treated, the eye that the brain ignores will never see well. This loss of vision is called amblyopia, also called “lazy eye”. Sometimes amblyopia appears first and causes strabismus.
In most children with strabismus, the cause is unknown. In more than half of these cases, the problem is present at birth or shortly thereafter, which is called congenital strabismus.
Most often, the problem has to do with muscle control and not muscle strength.
Other disorders associated with strabismus in children include:
• Apert Syndrome
• Cerebral palsy
• Congenital rubella
• Hemangioma near the eye during lactation
• Pigmentary incontinence syndrome
• Noonan Syndrome
• Prader-Willi Syndrome
• Retinopathy of prematurity
• Retinoblastoma
• Traumatic Brain Injury
• Trisomy 18
Strabismus in adults can be caused by:
• Botulism
• Diabetes (causes a condition known as acquired paralytic strabismus)
• Graves disease
• Guillain-Barré syndrome
• Eye injury
• Shellfish poisoning
• Stroke
• Traumatic Brain Injury
• Loss of vision due to any disease or eye injury
A family history of strabismus is a risk factor. Farsightedness may be a contributing factor, especially in children. Any other condition that causes loss of vision can also cause strabismus.
Symptoms
Symptoms of strabismus may be continually present or may come and go. They include:
• Crossed eyes
• Double vision
• Eyes that do not align in the same direction
• Uncoordinated eye movements (eyes do not move together)
• Loss of vision or perception of depth
It’s important to note that because children can develop amblyopia so quickly, they might never experience double vision.

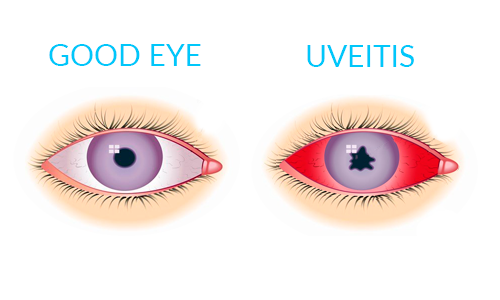
It is the swelling and irritation of the uvea, the middle layer of the eye that provides most of the blood supply to the retina.
Causes
Uveitis can be caused by autoimmune disorders such as rheumatoid arthritis or ankylosing spondylitis, infections or exposure to toxins. However, in many cases the cause is unknown.
The most common form is anterior uveitis, which involves inflammation of the front part of the eye. It is often called iritis because it usually only affects the iris, the colored part of the eye. Inflammation may be associated with autoimmune diseases but most cases occur in healthy people. The disorder may affect one eye only and is most common in young and middle-aged people.
Posterior uveitis affects the back of the uvea and primarily involves the choroid, a layer of blood vessels and connective tissue in the middle of the eye. This type of uveitis is called choroiditis and if the retina is also involved it is called chorioretinitis. You may develop this condition if you have had a body-wide infection or if you have an autoimmune disease.
Another form of uveitis is pars planitis, an inflammation that affects the narrow area (pars plana) between the colored part of the eye (iris) and the choroid. Pars planitis usually occurs in young men and is not generally associated with any other condition. However, some evidence suggests it may be linked to Crohn’s disease and possibly multiple sclerosis.
Uveitis can be linked to any of the following conditions:
• AIDS
• Ankylosing spondylitis
• Behcet Syndrome
• CMV retinitis
• Herpes zoster infection
• Histoplasmosis
• Injury
• Kawasaki disease
• Psoriasis
• Reactive arthritis
• Rheumatoid arthritis
• Sarcoidosis
• Syphilis
• Toxoplasmosis
• Tuberculosis
• Ulcerative colitis
Symptoms
Uveitis can affect one or both eyes. Symptoms may develop rapidly and can include:
• Blurry vision
• Floating spots in the vision
• Eye pain
• Redness of the eye
• Sensitivity to light